Tiny robots, giant steps: how nanotechnology could improve cancer and fertility treatment
An advanced robotics lab at Canada’s top university is helping the medical world tackle some of its most perplexing problems – starting at the smallest of scales
This article was originally published on theguardian.com as part of the University of Toronto and Guardian Labs What’s Possible? Ask Toronto campaign.
Advances in treatment and earlier detection have significantly improved cancer survival rates in recent decades. But some cancers remain devastatingly lethal. For patients with glioblastoma (GBM), the most common and aggressive form of brain cancer, the average life expectancy is just 12 to 18 months after diagnosis. Only a quarter will survive more than a year, and just 5% more than five years.
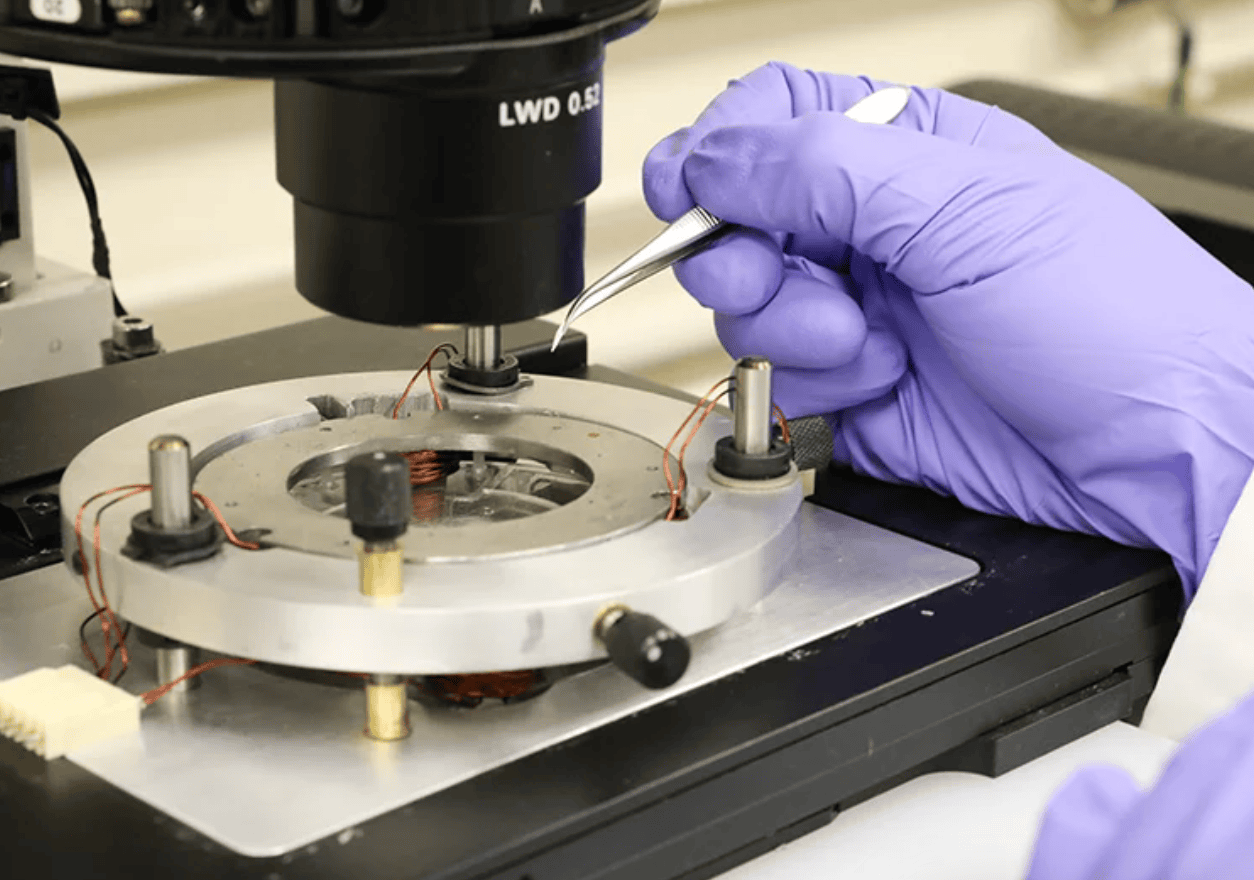
At the University of Toronto, Prof Yu Sun and his team at the Robotics Institute are harnessing the potential of nanorobotics – the field of technology developing microscopically small robots – to build what could be a game changing new treatment option: “nano-scalpels” that seek out cancer cells and destroy them by spinning when activated by a magnetic field.
While chemotherapy is an effective treatment for cancer in the beginning, patients eventually develop resistance to it, and in glioblastoma that happens quickly, says Sun, the founding director of the Robotics Institute. “We hope to give a resort to cancer patients having treatment resistance: can we give them some hope to treat their disease?” he says.
For Sun, the research has a personal resonance: he lost his mother to cancer, and saw first-hand the impact of treatment resistance. “I realised more acutely that patients really need technologies that can help them as the last resort,” he says.
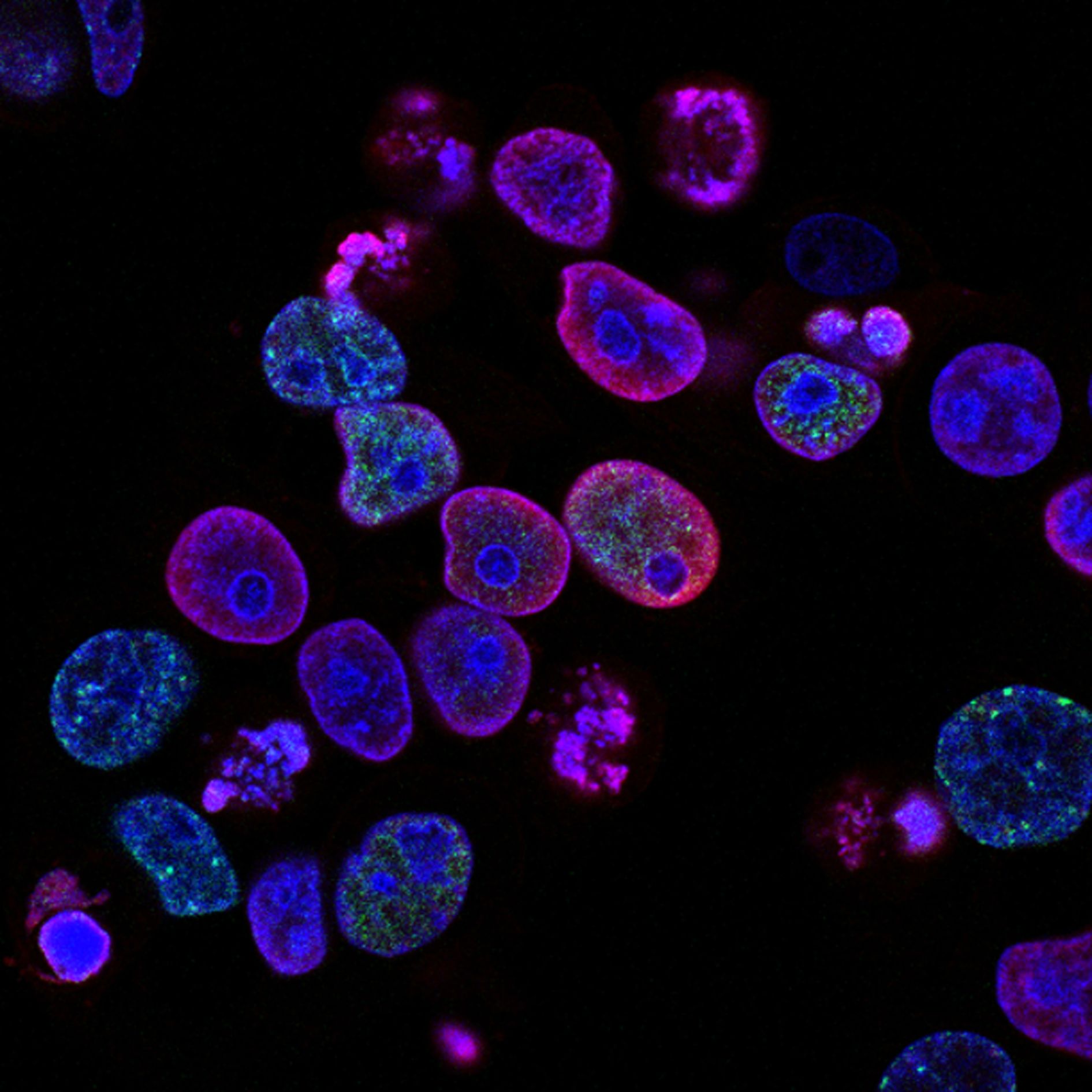
Working with Dr Xi Huang’s lab from Toronto’s Hospital for Sick Children (SickKids), the University of Toronto team developed their “mechanical nanosurgery” by filling magnetic carbon nanotubes – tubular molecules made of carbon – with iron oxide particles and coating them with an antibody that recognises a protein overexpressed by GBM tumour cells. Thanks to the antibodies, when the tubes are injected into a tumour, they seek out cancer cells. Then a precisely applied external rotating magnetic field makes the tubes spin.